The healthcare industry is under constant pressure to improve operational efficiency, reduce costs, and maintain compliance. One of the most time-consuming processes for hospitals, insurers, and healthcare providers is claims processing. Manual handling of claims not only delays reimbursements but also increases the risk of errors, fraud, and regulatory non-compliance.
This is where Robotic Process Automation (RPA) comes into play. By leveraging smart automation, healthcare organizations can streamline claims management, reduce turnaround times, and enhance patient satisfaction. Cross platform mobile app development services Dallas and android mobile app development services Dallas further complement RPA by enabling mobile access for staff and patients alike, enhancing real-time monitoring and operational efficiency.
Why Healthcare Claims Processing Needs Automation
Healthcare claims processing involves multiple steps:
- Verification of patient and policy information
- Cross-checking treatment codes with insurance coverage
- Submitting claims to payers
- Tracking approvals and rejections
- Managing follow-ups and audits
Manual processing of these steps often leads to delays, missed claims, and compliance risks. According to industry reports, healthcare providers lose billions annually due to inefficiencies in claims management. RPA solutions for faster claims processing help automate repetitive tasks, enforce rule-based workflows, and ensure accurate documentation.
Benefits of RPA in Healthcare Claims Processing
1. Accelerated Claims Processing
RPA bots can automatically extract data from claim forms, validate it against insurance policies, and submit it to payers. This reduces the average processing time from weeks to days or even hours.
Example: A Dallas-based health insurance provider implemented RPA to automate initial claim verification and reduced processing time by 70%, enabling faster reimbursements to patients.
2. Improved Accuracy and Compliance
Errors in claims processing can lead to denials, financial losses, and regulatory penalties. RPA ensures precision in data entry, code validation, and documentation. By maintaining detailed logs, it also simplifies auditing and compliance management.
Healthcare organizations can implement digital agri-insights-like monitoring frameworks for healthcare claims. While these tools are commonly used in agriculture for predictive analytics, similar AI-driven monitoring and verification can enhance claims accuracy.
3. Reduced Operational Costs
Manual claims processing requires extensive labor. By automating repetitive tasks, healthcare organizations reduce labor costs and redirect staff to more strategic functions such as patient care and policy review.
Example: A large hospital network in Dallas automated the claim adjudication process with RPA, reducing costs associated with manual processing by 50%.
4. Enhanced Fraud Detection
RPA combined with AI and analytics can flag unusual patterns in claims, such as duplicate submissions or inconsistent coding. Automated field monitoring and vision-based farming tools from agriculture inspire similar frameworks in healthcare, where pattern recognition and anomaly detection play a critical role.
5. Integration with Existing Healthcare Systems
RPA integrates seamlessly with EMR/EHR systems, billing software, and insurance platforms. Bots can pull patient data, cross-check it with policy information, and update records automatically. This unified ecosystem enhances efficiency and reduces the risk of data fragmentation.
Real-World Examples of RPA in Healthcare
- UnitedHealth Group: Uses RPA to automate claims processing, eligibility verification, and billing reconciliation, reducing errors and improving customer satisfaction.
- Cigna: Implements bots for claim adjudication and auditing, allowing faster reimbursements and accurate reporting.
- Blue Cross Blue Shield: Employs RPA solutions to handle high volumes of claims while maintaining strict compliance with healthcare regulations.
These examples show that automation is not just about efficiency—it is about transforming the patient and provider experience in a measurable way.
Technologies Enabling Smart Healthcare Automation
Advanced automation in healthcare often leverages AI and machine learning. Interestingly, technologies like computer vision agriculture apps, crop yield prediction AI, and precision agriculture CV tools inspire frameworks for data recognition, pattern analysis, and workflow optimization in healthcare claims.
By adopting AI crop analytics methodologies, healthcare providers can implement:
- Smart yield forecasting for claim approvals and financial planning
- Automated field monitoring analogs in claim validation
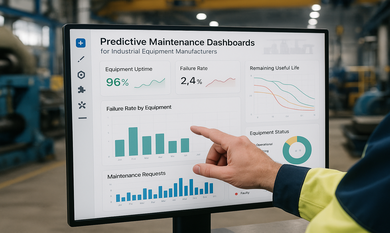
- Digital agri-insights-style dashboards for real-time analytics and reporting
Partnering with a computer vision software development services Dallas team ensures these intelligent automation solutions are seamlessly implemented. Similarly, integrating cross platform mobile app development services Dallas allows staff and administrators to monitor workflows, manage approvals, and generate reports on-the-go.
Implementation Strategies for Healthcare Startups and Providers
- Identify Repetitive Claims Processes: Focus on verification, submission, auditing, and reporting tasks that are rule-based and time-consuming.
- Choose the Right RPA Platform: Platforms like UiPath, Automation Anywhere, or Blue Prism provide enterprise-ready RPA solutions.
- Integrate with EMR/EHR Systems: Bots should pull patient data from existing systems and ensure compliance with HIPAA and other healthcare regulations.
- Leverage Analytics: Use dashboards to monitor bot performance, identify bottlenecks, and optimize workflows continuously.
- Scale Gradually:
Conclusion
RPA is revolutionizing healthcare claims processing by making it faster, more accurate, and compliant. Theta Technolabs, a leading provider of Web, Mobile and Cloud solutions, helps healthcare providers and startups implement scalable RPA strategies. With expertise in computer vision software development services Dallas, we deliver intelligent automation solutions that enhance operational efficiency, reduce costs, and improve patient satisfaction.
Transform Your Healthcare Claims Processing Today
For consultation or to implement intelligent RPA solutions in your healthcare organization:
📧 Email us: sales@thetatechnolabs.com
FAQs
1. What is RPA, and how does it help healthcare claims processing?
RPA (Robotic Process Automation) automates repetitive, rule-based tasks like data extraction, claim verification, and submission, reducing errors and speeding up reimbursements.
2. How does RPA improve compliance in healthcare?
RPA maintains detailed audit trails, enforces standardized workflows, and ensures that all claims are processed accurately according to HIPAA and other regulations.
3. Can RPA reduce operational costs for healthcare providers?
Yes. By automating repetitive tasks, hospitals and insurance providers save on labor costs and allow staff to focus on patient care and complex decision-making.
4. Which healthcare processes are ideal for RPA automation?
Claims verification, adjudication, billing reconciliation, fraud detection, and reporting are prime candidates for RPA automation.
5. How quickly can a healthcare organization implement RPA?
Implementation depends on the complexity of existing workflows. Many hospitals and insurers can automate specific processes within weeks, while full-scale adoption may take a few months.






















_Choosing%20the%20Right%20App%20Development%20Company_%20A%20Comprehensive%20Guide_Q1_24.jpg)
_Chatbots%20for%20Event%20Management%20and%20Hospitality%20Services_Q1_24.jpg)
_Best%20iOS%20App%20Development%20Company_%20Enhancing%20User%20Engagement%20with%20Push%20Notifications_Q2_24.jpg)
_Key%20Trends%20in%20Healthcare%20Software%20Development%20for%20the%20Future_Q2_24.jpg)
_How%20much%20does%20it%20cost%20to%20create%20an%20android%20app%20in%202024%20for%20Startups_%20A%20detailed%20guide_Q2_24.jpg)
_Integrating%20Chatbots%20Into%20Your%20Application.jpg)


_Enhancing%20Driver%20Safety%20and%20Compliance%20with%20Web%20Apps%20in%20the%20Logistics%20Sector_Q3_24.jpg)
_Web%20Apps%20for%20Retail%20and%20eCommerce_%20Streamlining%20Operations%20and%20Reducing%20Costs_Q3_24.jpg)
_How%20AI%20is%20Enhancing%20Construction%20Site%20Surveillance%20and%20Security%20in%20Dallas_Q3_24-1.jpg)
_The%20Impact%20of%20Cross-Platform%20Apps%20on%20Real%20Estate%20Market%20Trends%20in%20Dallas_Q3_24-1.jpg)
_Streamlining%20Appointment%20Scheduling%20with%20Cloud%20Computing%20in%20Dallas%20Healthcare_Q4_25.jpg)
_How%20Cloud%20Solutions%20Are%20Enhancing%20Remote%20Patient%20Monitoring%20in%20Healthcare_Q4_25.jpg)































.png)










.png)

.png)
.png)
.png)
.png)


.png)
.png)
.png)

.png)






.png)
.png)